Yes, it is as bad as you heard.
Yes, I do have PPE (personal protective equipment).
No, I have not had a patient die yet.
Yes, I have seen deceased patients.
 I am a med - surg nurse joining the Covid crisis fight in NYC. My face is breaking out from the mask tight against it 24/7 except in my hotel room. My nose is beginning to blister from the mask. I am drenched, dripping sweat the entire 13 hr shift. I never know where to find anything supply wise. My patients have no pillows. Some of them do not even have an incentive spirometer so I have been improvising and teaching them exercises to help their lungs. Med surg rooms don't have any monitoring, there is no capability for continuous oxygen monitoring. Most rooms do not even have a clock on the wall to count patient respiration and I cant look at my watch because I have 2 isolation gowns on with gloves. They make a point to open every single door and lay eyes on every patient from the doorway during report as patients have been found dead when the nurse entered the room.
I am a med - surg nurse joining the Covid crisis fight in NYC. My face is breaking out from the mask tight against it 24/7 except in my hotel room. My nose is beginning to blister from the mask. I am drenched, dripping sweat the entire 13 hr shift. I never know where to find anything supply wise. My patients have no pillows. Some of them do not even have an incentive spirometer so I have been improvising and teaching them exercises to help their lungs. Med surg rooms don't have any monitoring, there is no capability for continuous oxygen monitoring. Most rooms do not even have a clock on the wall to count patient respiration and I cant look at my watch because I have 2 isolation gowns on with gloves. They make a point to open every single door and lay eyes on every patient from the doorway during report as patients have been found dead when the nurse entered the room.
A day in the life:
- Walk 20 min to the hospital and go straight to the nursing office to obtain my assigned location for the day (every single day) and sign in.
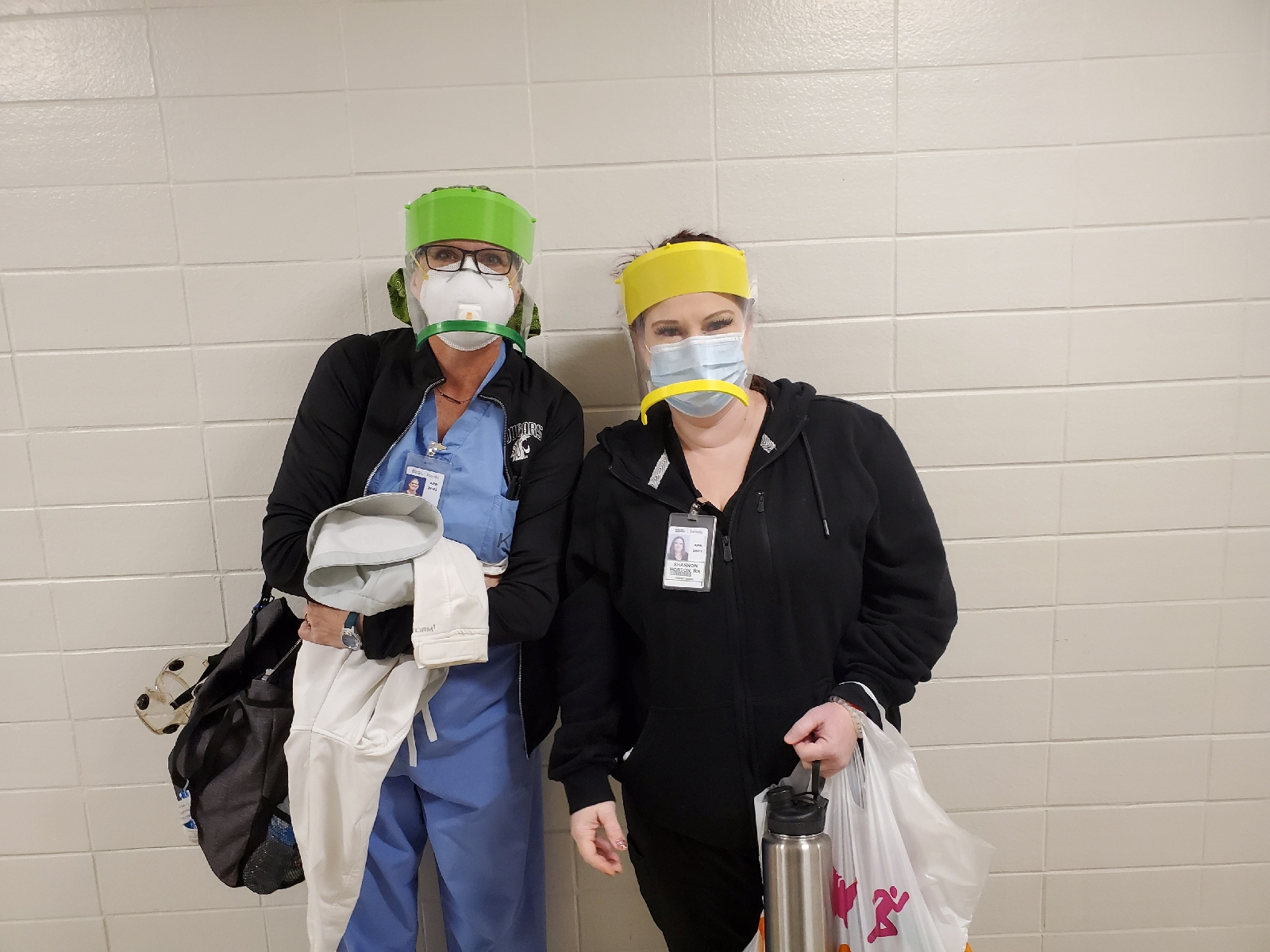
- Head to one of designated locations where a bag with one surgical mask and one N95 mask are provided to each staff member as they sign a form stating they have received the masks. This is the only way to get an N95 mask. Most units have boxes of disposable plastic isolation gowns, hair nets, boot covers, surgical masks, surgical masks with connected face shields, and gloves. Permanent hospital staff seems to have thick disposable isolation scrubs they get from somewhere and they wear these all day, removing only to go home at night.
- Find your way to your assigned unit and hope with fingers crossed it is NOT an intensive care unit and that you have no patients that are too critical for your skill set and assigned floor. Usually after 7am until all this is completed....
- Get your garb on-- most important step, no one hurries this or skips this. Often happens before they even consider getting report
- Get your assignment and hope (and pray) that they don't change staffing and send you to another unit within the first 2hrs of your shift since you already have report on these patients. They are apt to do this as they discover some units only have one nurse etc.

Garb for the day:
- scrubs worn from home, no layering/ bare minimum as hospital is quite hot and I know what else I will be wearing.
- disposable scrub set (usually only permanent staff have this)/ sterile thick surgical gown. This is worn over scrubs from first getting to unit until leaving in the evening.
- masks (yes plural)- first your N95 then a surgical mask over it as you may need to reuse the same n95 multiple days. (thankfully, I have not yet had to reuse, but am saving them just in case). Some nurses I met have been wearing the same n95 for a week solid and were told by nursing office they had to do this.
- Hair net and shoe covers
Now I am ready to get report. When preparing to go into a room, I don additional garb:
- plastic isolation gown (so hot, keeps body heat in)
- gloves
- additional surgical mask with connected face shield or...
- additional surgical mask + plastic face shield worn on head.
- some ppl have goggles instead of the face shields - point is eye protection
Upon leaving the patient room, the outer mask, gloves, and gown are discarded. If a separate face shield is worn, this is cleaned and used all day long (these are like GOLD and are very rare to find). If there are not any face shields and there is only a few masks with face shield attached, then you keep that outer mask with shield until you are done seeing patients for a bit.


I have been overwhelmed with the appreciation from my patients, the desk staff and the hotel, the lady setting up to go breakfast bags for nurses in the hotel, the nurses at the hospital, and people in the grocery store. My patient told his mom on the phone that he had an awesome nurse from Ohio and that he may get discharged home soon. His mom was tearful and saying thank you thank you for taking care of my son. Some units have received meal donations for medical staff and this made my day as I had packed a peanut butter and jelly sandwich. One unit charge nurse walked around the unit about 4pm with a bag of snacks, candy bars, and cloth masks which her friends had donated to the unit for a pick me up.
As of now, I have not coded or had a patient die, but the other nurses here at my hotel that I met have all had both of the above happen multiple times. There are not enough IV pumps, feeding pumps, or anything really. One colleague reported giving blood by drip without a filter because there was none available. I had 2 patients who needed NG feeds to be able to be one step close to discharge. After 24hrs, there was still no feeding pump available and the attending urged me to try whatever I could come up with to get some formula running.


I included pictures of a contraption I rigged up to administer based on calculated drips per min and titrated as ordered to achieve certain mls/hr. The first couple ideas didn't work and leaked, but I got a good system in the end. Pleased to say the patient was off feeds in 2 days and transitioned to regular food and on room air as he had tolerated feeds and his bipap so well. The staff and doctors loved it and I set it up for another two patients in similar situations. I took a tube feeding set, cut the tubing off from bag and discarded tubing. I then used IV tubing (as it had a roller clamp and packaging states 15 drops/ml) and spiked the feeding bag. The next problem was that the NG was a tube that could be vented and fed through not just a normal tube that can only feed so the opening was wide and needed something wedged in. I thought maybe using a foley cath would be a good connector. I cut the IV tubing end that screws into and IV off and discarded. I then stuck the foley into the NG and the end of the IV tubing into the foley to connect it all and provide enough of a seal that it would not leak. I then calculated the number of drops per minute and through trial and error used the roller clamp to get as close as possible to the ordered rate.

Every evening I am exhausted and sore when I finally arrive back to my hotel room, but it is the best moment of the day because I can finally take off the mask and breathe!! My face can get some air! I try to call my mom or text her as she begins to worry if she hasn't heard from me in 24hrs. I have people here checking on me as well. When I had to work on a day my friends were off, they texted to make sure I made it home and another time they walked to the hospital just to walk me home and ensure I was safe.
I have met some other amazing nurses from other states and thankfully have been able to walk back and forth to the hospital with a few on most days. We have made a routine of stopping just before walking in and taking a few minutes to pray before we walk into utter caos.

 Week four brought some changes. My walk to and from work buddy got moved from my hotel to a different hotel. We have been walking the 20 minutes to and from work on the days we both work. We made a routine of stopping to pray before we get to the hospital to begin our shift. On the bright side, I got some buttons in a package from my mom and was able to sew them onto the headband to protect my ears. I also ordered a scrub hat from Amazon (and it came surprisingly quickly) along with the 2 scrub hats I received from my friend's donations (one was pictured in a previous post) and I was able to sew buttons onto those hats as well to keep pressure off my ears.
Week four brought some changes. My walk to and from work buddy got moved from my hotel to a different hotel. We have been walking the 20 minutes to and from work on the days we both work. We made a routine of stopping to pray before we get to the hospital to begin our shift. On the bright side, I got some buttons in a package from my mom and was able to sew them onto the headband to protect my ears. I also ordered a scrub hat from Amazon (and it came surprisingly quickly) along with the 2 scrub hats I received from my friend's donations (one was pictured in a previous post) and I was able to sew buttons onto those hats as well to keep pressure off my ears.
 I had a talk with a friend last night, and she shared how my story has affected her. She said to me "Laura you are literally being the hands and feet of Jesus." This really stopped me in my tracks as I reflected on this and our conversation. I hope that the nurses and patients I come into contact with are uplifted by my reflection of Christ. In rooms with patients who have no family at their side while they are scared and sick, I can be there and love and encourage them.
I had a talk with a friend last night, and she shared how my story has affected her. She said to me "Laura you are literally being the hands and feet of Jesus." This really stopped me in my tracks as I reflected on this and our conversation. I hope that the nurses and patients I come into contact with are uplifted by my reflection of Christ. In rooms with patients who have no family at their side while they are scared and sick, I can be there and love and encourage them.